Authors: Nay Htyte MD, FACC, Back Kim, MD FACC, Esad Vucic, MD, Taean Choi ANP – the HEARTVEINNYC Team
Heart Vein NYC, New York, New York
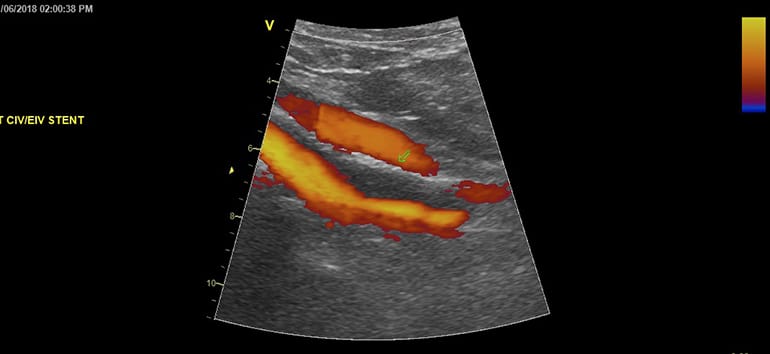
Percutaneous balloon venoplasty with stent placement for iliocaval obstruction has increasingly become a primary treatment option with excellent outcome showing almost immediate relief of clinical symptoms attributable to iliac vein compression.
Despite this clinical success, acute and subacute stent thrombosis rates (within 7d and 30d respectively) have had varied reports in current published data, and reliable large studies to establish this data are lacking.
Furthermore, a clear and standardized recommendation for anticoagulation or antiplatelet for stent patency has not been well established.
While the role of antiplatelet therapy in prevention of platelet activation and subsequent stent thrombosis is more commonly practiced with some practical standards in arterial and coronary angioplasty, the pathophysiology of thrombogenesis and the larger size of stents in the in the venous system (iliocaval veins) make clinically significant impact of effective antiplatelet inhibition in preventing venous stent thrombosis uncertain. There are studies that describe using only antiplatelet therapy in various combinations while others recommend aggressive anticoagulation therapy.
We hope to establish a statistically significant impact on decreasing early stent thrombosis rates with a combined antiplatelet and anticoagulation regimen without a significant increase in major and minor bleeding events.
In our experience, single antithrombotic therapy has seen some limitation in preventing clinically significant stent thrombosis during the immediate post-stenting period by showing an increasing trend towards the occurrence of subacute in-stent thrombosis (1-3 months).
In lieu of shortage of evidence and standardized recommendations on optimal medical regimen for effective prevention of venous stent thrombosis, we propose a combined antiplatelet and antithrombotic medications with a lead uploading of antiplatelet with P2Y12 inhibitor (clopidogrel 75 mg) and Xarelto low dose (15 mg) anticoagulation for 1 to 6 months then switching to a single aspirin 81mg alone indefinitely thereafter to prevent this newly observed rising trend in iliac vein stent thrombosis in the acute postprocedural period.




