Authors: Esad Vucic MD, Back Kim MD, Nay Htyte MD & Tae An Choi, ANP-BC
Heart Vein NYC, New York, New York
56 year old Hispanic male presented with a history of two weeks intermittent anginal chest pain.
He has a history of known coronary artery disease and underwent percutaneous coronary intervention in 2008 (The coronary anatomy of the patient was not known on presentation).
Additionally, the patient has a medical history of hyperlipidemia and hypertension. Current medications were: Aspirin 81 mg and Valsartan/Hydrochlorothiazide 80 mg/12.5 mg. Vital signs were except for a mildly elevated baseline heart rate of 96 beats per minute, unremarkable. The baseline electrocardiogram (Figure 1) demonstrated: normal sinus rhythm, anteroseptal and inferior Q wave changes with slow R wave progression. The electrocardiogram finding was consistent with a large prior myocardial infarction.
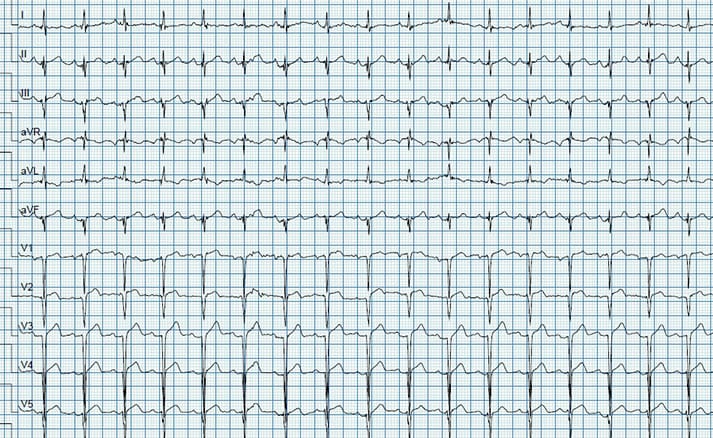
(Figure 1) The baseline electrocardiogram demonstrated: normal sinus rhythm, anteroseptal and inferior Q wave changes with slow R wave progression. The electrocardiogram finding was consistent with a large prior myocardial infarction.
To rapidly risk stratify the patient, he underwent cardiac stress testing with a standard Bruce protocol exercise treadmill stress test. Upon two minutes of exertion, the patient experienced mid-sternal chest pain and developed new anteroseptal ST-segment elevation in Lead V1-V4 (Figure 2, 3).

The stress test was immediately stopped and emergency medical services were called. The patient was at the same time brought onto a stretcher, IV access was obtained and a bedside echocardiogram was performed which revealed anterior apical hypokinesis and an estimated left ventricular ejection fraction of 35 %. The patient was then loaded with Brilinta and given 325 mg Aspirin and 50 mg Metoprolol. The patient’s vital signs were stable throughout and his chest pain resolved within a short time frame. EMS services arrived and he was brought to the nearest Hospital for further evaluation and treatment.




