Authors: Tae An Choi ANP-BC, Back Kim MD, FACC, and Nay Htyte MD, MSc., AACC
Heart Vein NYC, New York, NY
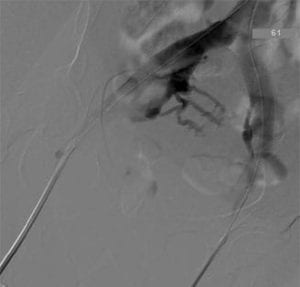 Percutaneous balloon venoplasty with stent placement for iliocaval obstruction has increasingly become a primary treatment option with excellent outcome. It is a minimally invasive and safe alternative choice to open surgical intervention (Palmer bypass). In a retrospective study of 304 limbs with symptomatic chronic venous insufficiency (CVI), the relief of iliac vein outflow obstruction with iliac vein stenting resulted in significant improvement of major symptoms of CVI and markedly restored quality of life (QOL)1. Linear results were observed in our patients. In our experience and as supported by numerous iliac vein stent literature, the potency of iliac vein stent is high with a low rate of in-stent stenosis and subsequent re-interventions. 2,3
Percutaneous balloon venoplasty with stent placement for iliocaval obstruction has increasingly become a primary treatment option with excellent outcome. It is a minimally invasive and safe alternative choice to open surgical intervention (Palmer bypass). In a retrospective study of 304 limbs with symptomatic chronic venous insufficiency (CVI), the relief of iliac vein outflow obstruction with iliac vein stenting resulted in significant improvement of major symptoms of CVI and markedly restored quality of life (QOL)1. Linear results were observed in our patients. In our experience and as supported by numerous iliac vein stent literature, the potency of iliac vein stent is high with a low rate of in-stent stenosis and subsequent re-interventions. 2,3
However, after the balloon venoplasty with stenting, the vein wall is potentially thrombogenic due to pressure injury from the deployment balloon and from the metallic stent. 4 Maintenance of stent patency requires either antiplatelet or anticoagulant medications. While the approach to anticoagulation with arterial stents is guideline-based, the optimal antithrombotic regimen has not yet been delineated and the superiority and inferiority among anticoagulant alone vs single antiplatelet therapy (SAPT) vs dual antiplatelet therapy (DAPT) vs combined anticoagulant + antiplatelet regimen have not been validated as well.
In our experience, either SAPT or DAPT is insufficient in the immediate post-stenting period (1-3 months) and is associated with an increased occurrence of subacute in-stent thrombosis. In this context, we employ therapeutic anticoagulation for 1 to 6 months using one of the novel anticoagulant agents (prophylactic dosage of rivaroxaban or apixaban) combined with a single antiplatelet and switch to a single antiplatelet alone thereafter with superior stent patency to SAPT or DAPT. The decision of the duration of anticoagulation therapy is made based on a degree of stenosis, length of stenosis, overlap of stents, complexity of disease, severity of fibrosis, post-thrombotic vs nonthrombotic iliac vein lesion (NIVL) and presence of thrombophilia.
Reference
- 1.Raju S. et al. The clinical impact of iliac venous stent in the management of chronic venous insufficiency. J Vasc Surg 2002;35;8-15
- 2.Raju. S Best management options for chronic iliac vein stenosis and occlusion. J Vasc Surg 2013;57:1163-9.
- 3.Garg N. et al. Factors affecting the outcome of open and hybrid reconstructions for nonmalignant obstruction of iliofemoral veins and inferior vena cavla J. Vasc Surg 2011:53:383-93
- 4.Tae An C. NP-BC, Back K. MD et al. Iliac Vein Compression Syndrome. Consultant 2017; Vol 12; Issue 57.




