Authors: Tae An Choi ANP-BC, Nay Htyte MD FACC, & Back Kim MD FACC.
Heart Vein NYC, New York, New York
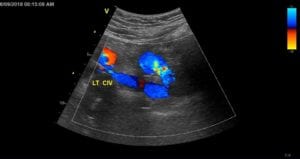 A 72-year-old male with a history of recurrent episodes of DVT in 2015 and 2017. First unprovoked DVT of left lower extremity in 12/2015, was treated with Xarelto for 6 months and 2nd DVT developed in 8/2017, he was hospitalized and re-started on Xarelto with improvement of pain and swelling until 12/2017, then it worsened while on anticoagulation. There was clinical and laboratory suspicion for multiple myeloma but no definite diagnosis. He underwent workup of hypercoaguable state which was negative. In 5/2018, he presented in Heart Vein NYC, for evaluation of severe left lower extremity pain and swelling with extensive venous stasis hyperpigmentation. Sonogram reveals chronic non-occlusive left sided femoral and popliteal DVT and severe narrowing of left common iliac vein (CIV) due to compression by right common iliac artery (CIA) (figure 1).
A 72-year-old male with a history of recurrent episodes of DVT in 2015 and 2017. First unprovoked DVT of left lower extremity in 12/2015, was treated with Xarelto for 6 months and 2nd DVT developed in 8/2017, he was hospitalized and re-started on Xarelto with improvement of pain and swelling until 12/2017, then it worsened while on anticoagulation. There was clinical and laboratory suspicion for multiple myeloma but no definite diagnosis. He underwent workup of hypercoaguable state which was negative. In 5/2018, he presented in Heart Vein NYC, for evaluation of severe left lower extremity pain and swelling with extensive venous stasis hyperpigmentation. Sonogram reveals chronic non-occlusive left sided femoral and popliteal DVT and severe narrowing of left common iliac vein (CIV) due to compression by right common iliac artery (CIA) (figure 1).
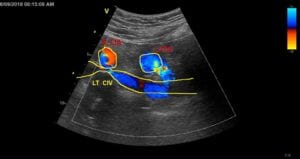 Figure 1 severely narrowed left CIV, compressed by right CIA at the venous-arterial crossing.
Figure 1 severely narrowed left CIV, compressed by right CIA at the venous-arterial crossing.
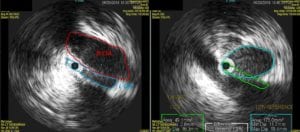 Figure 2 IVUS showing IVUS showing 71% luminal narrowing (green circle) compared to reference vessel size (blue circle)
Figure 2 IVUS showing IVUS showing 71% luminal narrowing (green circle) compared to reference vessel size (blue circle)
Intravascular ultrasound (IVUS) reveals extrinsic compression of left common iliac vein (CIV) from traversing common iliac artery (CIA), with over 71 % luminal reduction in diameter compared to adjacent normal reference segment (figure 2).
Balloon dilation with a stent deployment was successfully performed (figure 3).
 Figure 3. Venogram demonstrating balloon inflation followed by deployment of stent in left CIV
Figure 3. Venogram demonstrating balloon inflation followed by deployment of stent in left CIV
The subsequent intravascular ultrasound (IVUS) imaging shows a completed resolution of diffuse iliac vein compression by right CIA status post iliac vein stent implantation (figure 4).
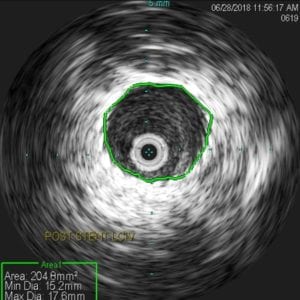
Figure 4. IVUS demonstrating decompressed left CIV after stenting.
Iliac vein stenting resulted in significant improvement in limb pain and swelling. With relief of orthostatic leg pain and achiness, patient returned to baseline normal daily activities.




